Managing the financial flow is as vital as delivering exceptional patient care in the healthcare sector. Revenue Cycle Management (RCM) stands at the forefront of this challenge, ensuring a seamless financial journey from patient appointment scheduling to the final payment collection. It’s a strategic approach, a blend of administrative acumen and clinical efficiency, pivotal in driving healthcare providers toward fiscal stability and growth. Let’s dive into the essence of revenue cycle management, uncover its critical components, and explore how IBN Tech’s expertise can transform your financial operations.
Table of Contents
1. What is Revenue cycle?
2. Factors Affecting the Revenue Cycle
3. What is Revenue Cycle Management?
4. Revenue cycle management systems
5. The Benefits of Healthcare Revenue Cycle Management
6. Why RCM is Essential for Both Providers and Patients
7. Revenue Cycle Management FAQs
What is Revenue cycle?
Healthcare Financial Management Association (HFMA) defines the revenue cycle as the administrative and clinical tasks that contribute to capturing, managing, and collecting revenue.
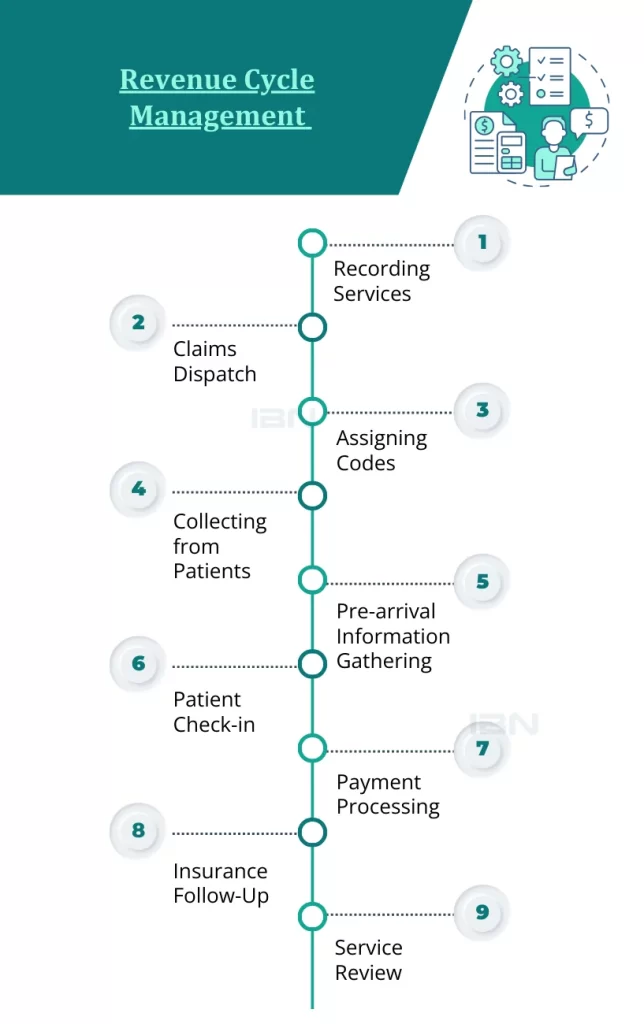
A revenue cycle looks like this:
- Recording Services: This step involves noting down the billable services provided to a patient. It’s about transforming medical services into billable charges.
- Claims Dispatch: This is the process of sending claims for billable services to insurance companies. The claims detail the services and their corresponding charges.
- Assigning Codes: This step involves attributing standard codes to the diagnoses and procedures. These codes are crucial for billing and statistical purposes.
- Collecting from Patients: This step is about identifying the amounts patients owe after insurance payments and collecting these amounts.
- Pre-arrival Information Gathering: This involves gathering preregistration information like insurance coverage before a patient arrives for inpatient or outpatient procedures. This step helps in confirming the patient’s insurance eligibility.
- Patient Check-in: This step involves gathering additional patient information during registration to create a medical record number and fulfill various regulatory, financial, and clinical requirements.
- Payment Processing: This involves processing payments through remittance processing. The payments received from insurance companies and patients are matched to the corresponding patient accounts.
- Insurance Follow-Up: This involves following up with third-party insurers to collect payments. This step becomes necessary when insurance companies delay or reject the payments.
- Service Review: This involves reviewing the necessity of medical services provided to a patient. This step is important in avoiding unnecessary medical procedures and managing healthcare costs.
Each of these steps is critical in the revenue cycle management process, ensuring that healthcare providers receive accurate and timely payments for their services.
Factors Affecting the Revenue Cycle?
Elements influencing the revenue cycle are both internal and external and common to financial considerations. Similar to other financial aspects, a healthcare organization has a degree of influence over internal dynamics like provider productivity, patient volume, and service fees. However, external factors such as patient payments and insurance claims reviews are more challenging to impact directly.
What is Revenue Cycle Management?
In healthcare, revenue cycle management is used to manage both the administrative and clinical aspects of revenue generation. This process begins as soon as a patient reaches out to schedule an appointment and concludes with the final payment for the services and treatments received.
The main goal of revenue cycle management is to identify and resolve any challenges in the provider’s revenue cycle. Through efficient RCM, healthcare providers can enhance their claim reimbursements and increase the revenue generated from patient services.
Revenue cycle management systems
Healthcare facilities often turn to specialized RCM systems to effectively manage and organize patient billing records. These systems play a vital role in bridging the divide between service delivery and payment collection. They achieve this by seamlessly integrating with diverse health systems, including electronic health records (EHR) and revenue cycle medical billing
systems. In doing so, they effectively track the patient’s journey throughout their healthcare experience.
RCM systems enhance operational efficiency by automating tasks traditionally performed manually. For instance, they handle administrative responsibilities such as notifying patients about upcoming appointments, alerting both payers and patients about pending balances, and engaging with insurance companies regarding claim inquiries or denials.
One significant advantage of RCM systems is their ability to mitigate financial losses by providing insights into the causes of claim denials. They prompt healthcare staff to ensure complete and accurate information for claim processing, reducing the need for claim revisions or resubmissions. This not only clarifies the reasons behind claim rejections but also guarantees appropriate reimbursements, particularly for Medicare services.
Organizations also leverage data analytics tools within these systems. By using dashboards, they can set, track, and adjust revenue goals, analyzing billing data to identify areas for improvement in their revenue cycles. This data-driven approach allows for the generation of detailed reports that guide strategic decision-making.
Modern RCM systems are increasingly incorporating advanced technologies like cognitive computing and robotic process automation. Cognitive computing ensures the accurate assignment of medical codes to patient records, while robotic process automation expedites various aspects of the revenue cycle, making the entire process more efficient and less prone to human error.
The Benefits of Healthcare Revenue Cycle Management
Effective management of the healthcare revenue cycle is a transformative force for healthcare providers, guaranteeing precise and meticulous execution of financial processes to navigate around delays and prevent revenue loss. However, the benefits of revenue cycle management go beyond merely augmenting provider income. They also encompass improvements in patient satisfaction, rendering RCM an indispensable asset in healthcare administration.
A Closer Look at RCM’s Numerous Perks:
Early detection of mistakes
RCM helps catch mistakes in medical bills, so claims don’t get rejected. This means less chance of errors like missing info or wrong codes. Getting it right the first time makes sure hospitals get paid quickly and saves money by avoiding fights over denied claims. Imagine a hospital making an extra $4-5 million just by fixing these mistakes early!
Less Paperwork, More Patient Focus
RCM reduces claim denials, meaning less work for the admin team. With fewer paperwork hassles, there’s more time to concentrate on taking care of patients. From setting up appointments to handling claims, RCM makes everything smoother and more enjoyable for everyone.
Guarding Against Fraud
RCM is like a superhero against healthcare fraud. It makes sure that billing and coding are accurate, lowering the risk of providing wrong information that could lead to costly investigations. It keeps healthcare providers updated on rules, protecting their good name.
Stopping Patient Fraud
RCM’s careful checks also help prevent fraud by patients. This includes mistakes in insurance details or someone pretending to be someone else. Finding and fixing these problems early protects both the healthcare provider and the patient from the consequences of fraud.
More Money for Better Care
Without technical issues, claim fights, and fraud worries, healthcare places get paid on time. This financial stability means healthcare providers can use the money to invest in giving the best possible care to their patients.
Why RCM is Essential for Both Providers and Patients
Revenue cycle management services
are crucial because they not only boost provider revenue but also enhance patient care. By minimizing time spent on administrative tasks, RCM allows healthcare providers to focus more on value-based patient care. This shift means better treatment and more efficient healthcare delivery.
IBN Tech stands out in the domain of revenue cycle management services, specifically excelling in medical billing and revenue cycle outsourcing. We set ourselves apart as more than just service providers; we serve as your committed financial health strategists, dedicated to enhancing your entire revenue cycle with precision, efficiency, and a compassionate touch.
As a leading player among revenue cycle management companies in the USA, IBN Tech is your reliable partner for healthcare bookkeeping services. We guarantee the highest levels of efficiency and effectiveness not only in medical billing but also in managing accounts receivable in the healthcare sector, ensuring comprehensive support for your financial operations.
Looking to transform your healthcare facility’s financial health with RCM? Let’s discuss your unique needs and craft a solution to fit them. IBN Tech is here to navigate the complexities of revenue cycle management for you. Connect with us now for a brighter, financially healthier tomorrow in healthcare.
Revenue Cycle Management FAQs
- Q.1 What is revenue cycle management in healthcare?
- Revenue cycle management (RCM) in healthcare refers to the financial process that healthcare facilities use to track patient care episodes from registration and appointment scheduling to the final payment of a balance.
- Q.2 What does revenue cycle management mean?
- Revenue cycle management means managing all aspects of the financial processes involved in patient care, including billing, collections, and patient financial services, to ensure that healthcare providers receive timely and complete payment for services rendered.
- Q.3 what does revenue cycle management mean?
- Revenue Cycle Management (RCM) is a strategic process used by healthcare providers to efficiently handle the capture, management, and collection of patient service revenue, from appointment scheduling to final payment collection.